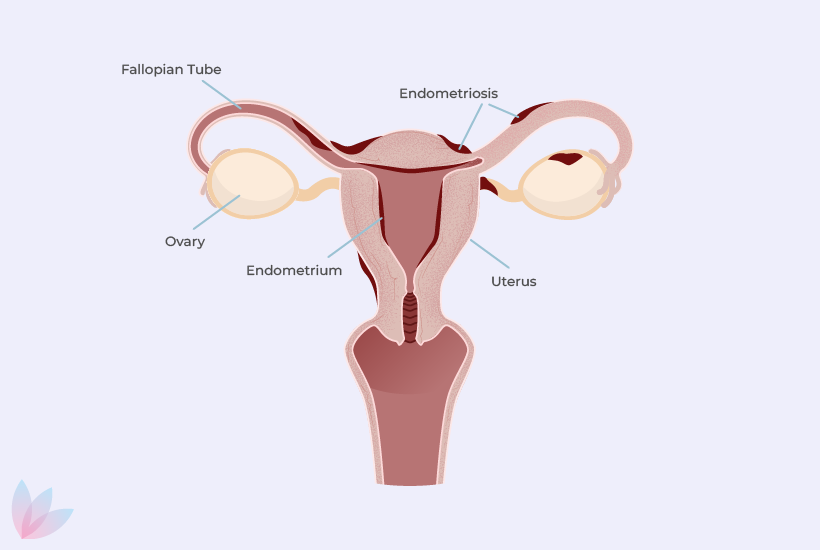
Endometriosis Treatment Options
Endometriosis is an evolving disease during the reproductive years but can be managed with a variety of medical, surgical and complementary treatments as well as lifestyle changes.
After the diagnosis of endometriosis we will discuss with you to explore and decide the most suitable treatment options, considering your specific circumstances.
There are several reasons for undergoing treatment for endometriosis, including pain and other symptoms relief, slowing down the growth of the disease, improving fertility and preventing the endometriosis from returning.